The Typical Job Description (and Why It’s Not That Helpful)
You’ve probably seen a description that sounds something like:
Pathologists’ assistants perform gross dissection and examination of surgical specimens. They also perform autopsies, both forensic and medical. They work under the indirect supervision of pathologists.
Or even better and more generic:
A pathologists’ assistant is a highly trained, certified allied health professional who is qualified by academic and practical training to provide services in anatomic pathology under the supervision of a licensed, board-certified, or board-eligible anatomic pathologist.
Services in both surgical and autopsy pathology include processing a variety of laboratory specimens, comprehensive macroscopic examination, and evaluating all surgical pathological specimens. Pathologists’ assistants also perform postmortem examinations including prosection, assisting the pathologist with rendering the provisional anatomic diagnosis, composing the clinical history, recording the macroscopic anatomic findings, and submitting tissue sections for microscopic examination.
While this technically isn’t incorrect, it leaves a lot to be desired.
Let’s start off with what is pathology and what a pathologist is before we can understand what it is a pathologists’ assistant (PA) does.
What Is Pathology, Anyway?
Pathology is the study and diagnosis of disease. This is accomplished by looking at tissues, fluids or organs removed through surgery and are generically referred to as “specimens”.
What Does a Pathologist Actually Do?
A pathologist is the physician that looks at these specimens. And they look in two different ways – one is zoomed out and the other is zoomed waay in.
Or you could imagine they
- Look at a specimen with their eyes

- Look at a portion of the specimen under a microscope
By looking at a specimen in these ways, they are able to identify areas of pathology, or where the disease is located.
They can also tell exactly what kind of disease it is, based on how the individual cells look. And if it’s a tumor, they can tell if it’s benign or malignant.
Benign = not cancer
Malignant = cancer
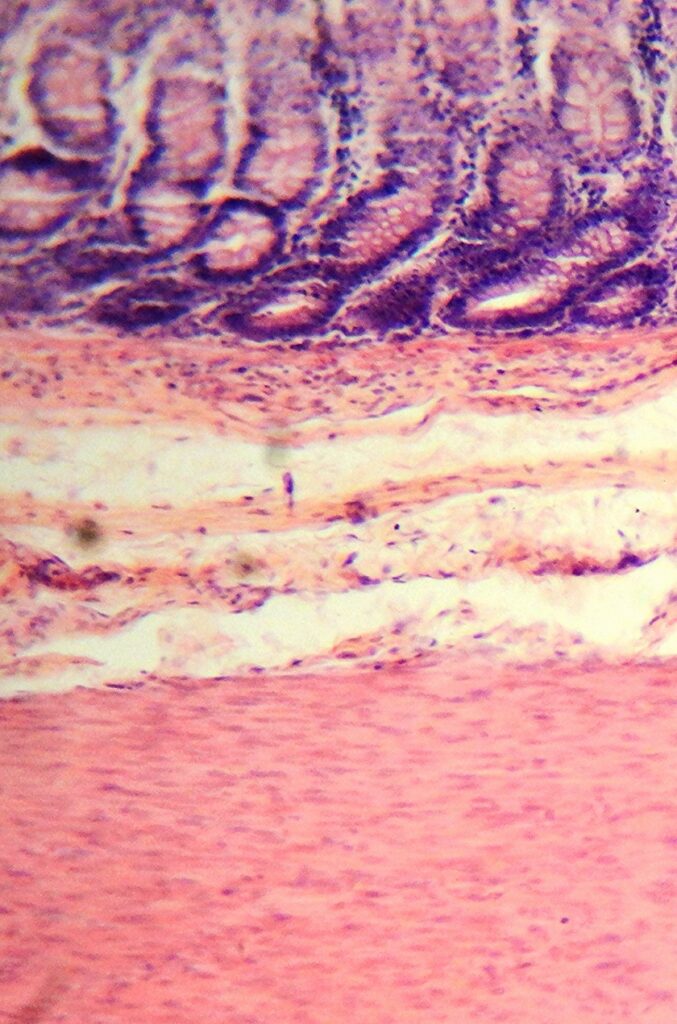
How Do They Look at the Cells?
But in order to tell this, the pathologist has to look at some of the cells from a specimen on a slide. The tissue on a slide is only a few microns thick to be able to show individual cells.
1 mm = 1000 microns
Even a relatively small piece of tissue will need to be cut in order to properly fit a slide.
Where the Pathologists’ Assistant Comes In
This is where a pathologists’ assistant comes in!
A PA trains to do several tasks that a pathologist can also perform, but their main role is to visually examine tissue, describe what they see, and then dissect it so it can be processed to ultimately fit on a slide. This process is called “grossing.”
Grossing
What is grossing?
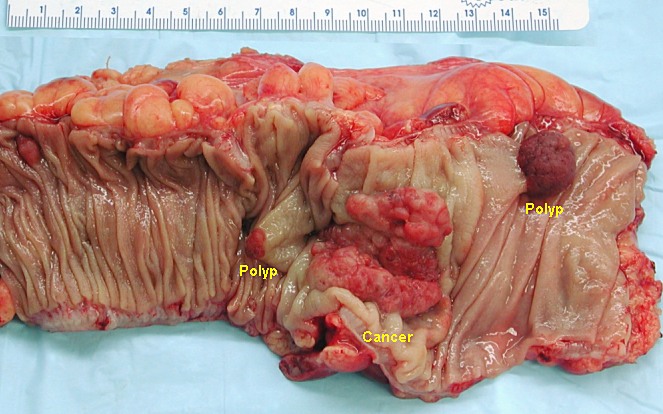
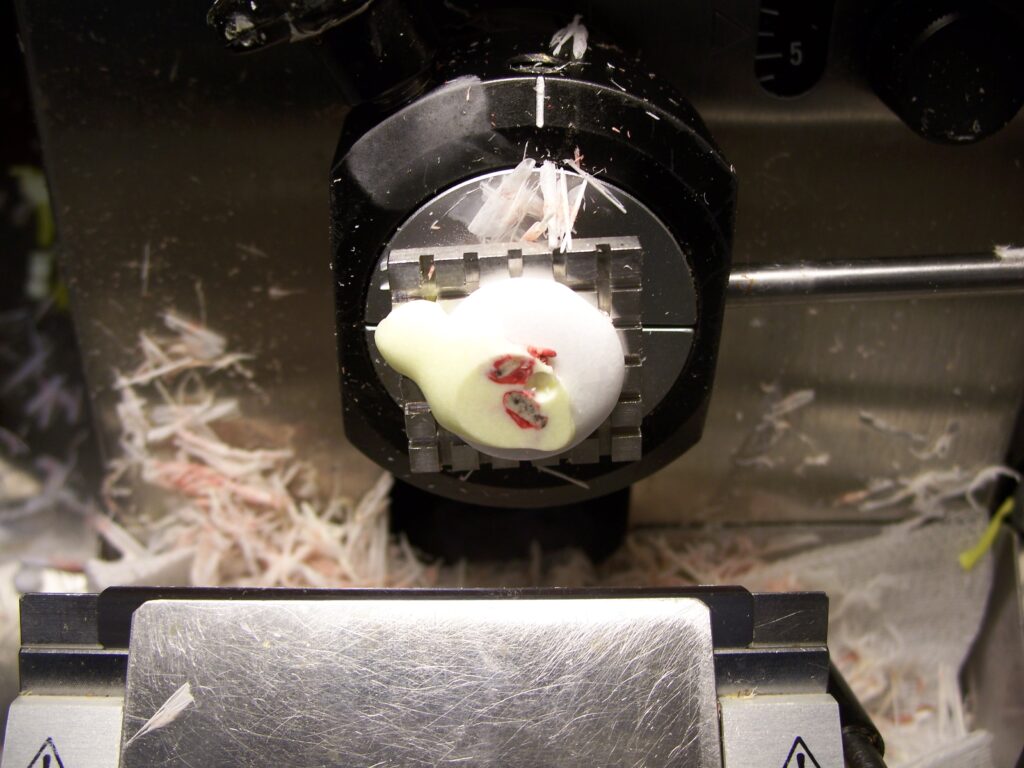
Grossing is the macroscopic (looking at tissue with your eyes) examination and description of surgically removed tissue. You’re looking for areas of disease (pathology), like the polyps and cancer in this picture.
Key Things a PA Identifies During Grossing
In grossing this specimen, a PA is able to identify several things.
- Type of specimen and surgery. If the surgeon said they removed a piece of colon, did you receive a piece of colon (or large intestine) in the lab or did you get a piece of small intestine? Sometimes miscommunications happen and we’re there to double check!
- Specimen orientation. Sometimes this is obvious but if it isn’t the surgeon will label the tissue for the lab. Is often provided with sutures (eg short superior, long lateral; or suture marks distal margin).
- Visible pathology. Is there a mass? Does it look bloodier or paler than normal?
- Size & depth of pathology? Size or extent of an area of pathology can affect staging if the pathology is a tumor.
- Surgical margin(s). Distance to the margin(s) tells the pathologist (and ultimately the surgeon who removed the tissue) if they removed all of the area of disease. Especially in cases where the disease might be cancer, the surgeon wants to remove all of it if possible for the patient.
Additional Tasks During Grossing
The PA can also do a few other things while grossing which can be helpful like:
- Taking and annotating photos
- Special testing (eg sending a sample for flow cytometry or microbiology)
Dissecting the Specimen
Finally after describing all of that and putting it into a report for the pathologist, a PA will dissect the specimen so they can see all of the cut surfaces and so they can prepare some of the larger specimen to be put onto a slide for the pathologist.
For very small pieces of tissue (eg a skin or colon biopsy) these might not need to be cut at all if they’re small enough for processing (“processing” here refers to everything that occurs after a PA handles the tissue in order for it to be put on a slide).
But for larger pieces of tissue, this part of grossing makes a big difference.
First of all, the area of pathology might be hiding in the specimen and won’t be visible on the surface or outside of the tissue. To find it and fully describe it, the PA will cut through the tissue. Also in cutting or slicing through the tissue, the PA is able to select representative pieces of that specimen to be turned into slides.
Submitting Tissue for Microscopy
Each of these white rectangles show where a PA might slice and submit pieces of the tissue. These “sections” of the tissue can show
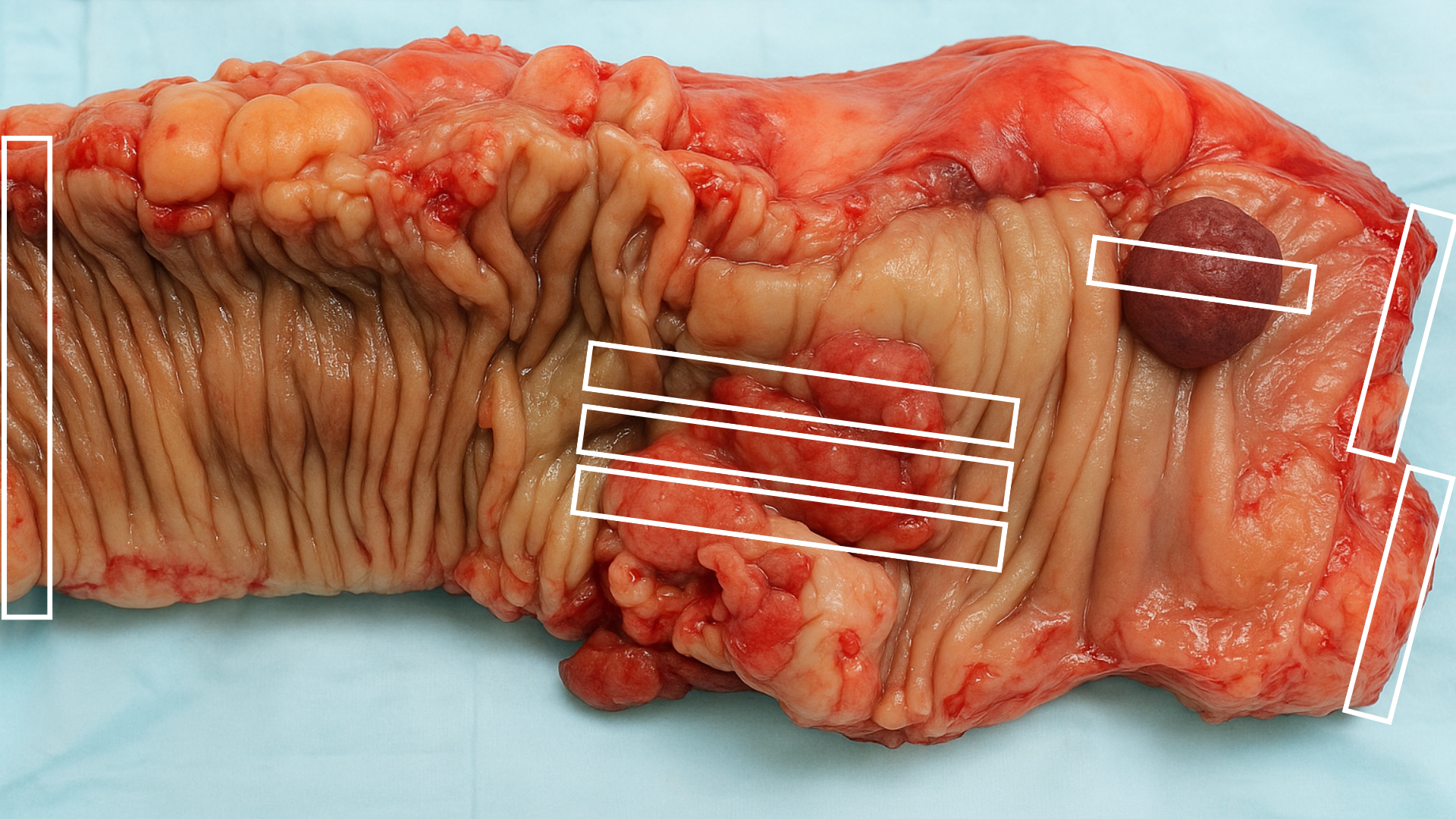
- The left and right edges of the tissue (or proximal and distal margins)
- The tumor in the middle (how big it is and how deep it goes)
- The polyp in the top right (which might be another tumor or it might just be a polyp that could eventually turn into cancer if it wasn’t removed)
Helping the Pathologist See the Full Picture
From those sections, a pathologist will see the most important representative pieces of the specimen on their slides. Along with the description of the tissue the PA already gave (also called a gross description – see an example of a gross description at the end of this post), the pathologist can tell the surgeon what kind of pathology they removed (eg often cancer but can also be something like inflammation), what stage/grade the tumor is if it is cancer and if the margins are clear of the pathology (aka did the surgeon remove it all?)
The PA is the eyes and ears (well, actually just eyes) of the pathologist and performs the gross examination in the lab so the pathologist can focus on the microscopic (or histologic) examination of those tissues.
Scope of Practice
Since a pathologists’ assistant is doing this work for a pathologist, technically a PA is under the supervision of a pathologist. PAs work independently but will ask for help when grossing if something is unusual, unexpected or if they’re just not sure how to handle something complicated.
And because the final diagnosis of any surgical specimen is based on histologic exam (aka looking at cells on slides), a PA does not diagnose anything. The final diagnosis is up to the pathologist.
Ok so what else does a pathologists’ assistant do?
Frozen Sections
Now that we know what a pathologists’ assistant does and what grossing is we can talk about frozen sections.
What Is a Frozen Section?
The normal grossing process takes 1-2 days and between someone going in for surgery and getting a final result from pathology, it can be several days before that entire process is complete and a diagnosis is given.
But what if a surgeon needs an answer about a specimen right away? Enter the frozen section.
When a surgeon requests a frozen section, they send a small portion of tissue to the pathology lab for rapid, real-time assessment during surgery. This helps guide immediate surgical decisions.
The Role of the Pathologist and PA
A pathologist and a pathologists’ assistant work together on the frozen section:
- The tissue is received fresh
- If it’s small enough, the entire sample is used. If not, just a representative piece is selected
- This selected piece is then prepared for rapid analysis
How the Tissue Is Processed
The tissue is:
- Frozen in a specialized device called a cryostat
- Sectioned into slices only a few microns thick
- Placed on a microscope slide

Manual Staining and Diagnosis
The PA stains the slide by hand to make the cells visible under the microscope.
The pathologist then immediately examines the slide and contacts the surgeon with the findings.
The entire process takes less than 20 minutes.
Based on the frozen section, the pathologist can tell the surgeon about:
- Whether the tissue appears benign or malignant
- If the surgical margin is clear of tumor
- Whether more tissue needs to be removed or if the surgery should continue
Limitations of Frozen Sections
While fast, frozen sections are not quite as accurate as standard tissue processing:
- Freezing can introduce artifacts that affect slide quality.
- The pathologist doesn’t have access to the full range of staining and diagnostic tools used in routine processing.
The PA’s Role in the Process
The pathologists’ assistant may:
- Perform the gross examination
- Select and prepare the tissue
- Handle the manual staining
- Prepare slides for the pathologist
Autopsy
Lastly, PAs are involved in autopsy.
Autopsy and the Pathologists’ Assistant
Not all pathologists’ assistants (PAs) perform autopsies, and for those who do, it’s usually a smaller part of the job compared to surgical grossing or frozen sections.
But when PAs are involved, their main role is in the evisceration—removing all of the internal organs for examination.

Autopsy and the Pathologists’ Assistant
Not all pathologists’ assistants (PAs) perform autopsies, and for those who do, it’s usually a smaller part of the job compared to surgical grossing or frozen sections.
But when PAs are involved, their main role is in the evisceration—removing all of the internal organs for examination.
Step 1: Consent and Identification
The autopsy process starts by verifying that proper consent has been obtained—usually from a close family member such as a spouse, parent, or child.
The PA and pathologist then identify the body together and determine what kind of autopsy is being performed based on the given consent. Some autopsies are complete, involving all organ systems, while others are limited to specific areas.
Step 2: External Examination
Next comes the external exam. Clothing and personal items are removed and stored to return to the body after the autopsy.
The PA records detailed observations, including:
- Height and weight
- Eye color
- Scars, tattoos, or other identifying marks
- Medical interventions (e.g., IV lines, bandages, catheter tubing)
- Any external injuries
Even life-saving efforts like CPR can result in broken ribs—and it’s our job to document everything.
Step 3: Internal Examination (Evisceration)
Once the external exam is complete and the patient history has been reviewed with the pathologist, the PA begins the internal portion of the exam.
Most autopsies begin with a Y-shaped incision to open the chest and abdomen. After removing the rib cage, the PA can access and remove all major organs—from the neck to the pelvis.
Step 4: Observations During Evisceration
As the organs are removed, the PA reports any abnormalities to the pathologist—things like:
- Unexpected holes or tears in tissue
- Unusual color changes in organs (eg darker or lighter than normal)
- Fluid or blood in the chest or abdominal cavity
These details can offer valuable clues about the cause of death.
Step 5: Organ Dissection
The removed organs are then given to the pathologist for further examination. Just like in surgical grossing, small sections are submitted to be processed and turned into slides.
Sometimes the cause of death is obvious during the evisceration or gross examination. Other times, slides are needed—and in rare cases, no definitive cause is found even after everything is reviewed.
Final Steps: Cleanup and Closure
Some tissue may be kept temporarily in case the pathologist needs to revisit their findings.
Most of the organs are then returned to the body, which is sutured closed by the PA. After cleaning the autopsy suite, the body is released for funeral home pickup.
Pingback: Pathologist vs Pathologists' Assistant - Canadian Path Assistant
Pingback: Pathologists’ Assistant vs. Physician Assistant: What’s the Difference Between the Two PAs? - Canadian Path Assistant
Pingback: Pathologists’ Assistant vs. Cytotech vs. Histotech
Pingback: Can Canadian Pathologists’ Assistants Practice in the United States? - Canadian Path Assistant
Pingback: How to Get Certified as a Pathologists’ Assistant in Canada - Canadian Path Assistant
Pingback: Tissue Fixation and Processing for Pathologists’ Assistants