What Are Colon Polyps?
Colon polyps are abnormal mucosal growths projecting into the lumen of the colon. They vary widely in:
- Shape (gross appearance)
- Histological features
- Risk of malignancy
These are common findings during colonoscopies and gross dissection of bowel specimens. Not all polyps are created equal – what are the gross differences and the malignant potential of each of them?
The most common neoplastic polyps are colonic adenomas, which are the precursors to the majority of colorectal adenocarcinomas (aka colon cancer). Colorectal adenomas are characterized by the presence of epithelial dysplasia. Typical adenomas range from 0.3 to 10 cm in diameter and can be pedunculated (think mushroom) or sessile (think flattened).
Gross Morphology: Sessile vs Pedunculated
Identifying differences in what polyps look like can tell you (and the pathologist) how likely they are to become cancerous. Recognizing these differences helps guide your sampling and can ultimately affect patient outcomes.
Sessile Polyps
Gross Features:
- Broad-based attachment directly on the mucosa
- Flattened, slightly elevated appearance
- May blend into the surrounding mucosa
Examples:
- Conventional adenomas
- Sessile serrated lesions (serrated = these have a sawtooth appearance histologically)
Malignancy Risk:
- Often higher than pedunculated polyps of the same size
- Harder to completely resect

Pedunculated Polyps
Gross Features:
- Have a stalk that connects them to the mucosal surface (like a mushroom)
- Project into the lumen of the colon
Examples:
- Tubular adenomas
- Some tubulovillous adenomas
Malignancy Risk:
- Generally lower than sessile polyps of the same size
- Risk increases with size and degree of dysplasia
Architectural Subtypes
Adenomas are further categorized histologically based on their glandular architecture:
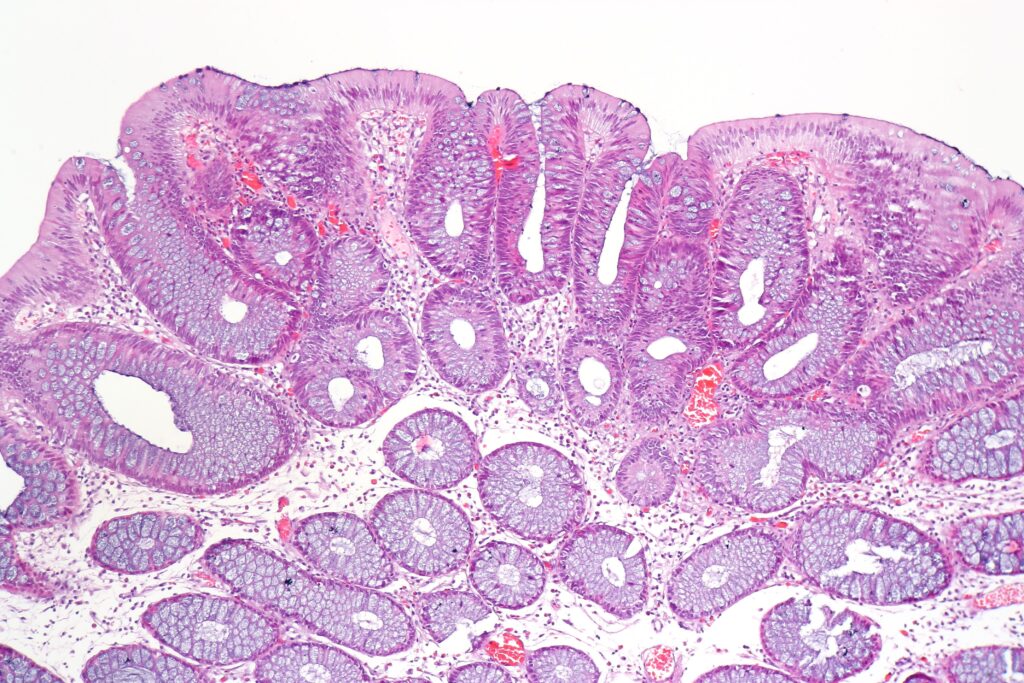
Tubular Adenomas
- Typically small and pedunculated
- Comprised mostly of tubular glands
- Malignancy risk: Relatively low
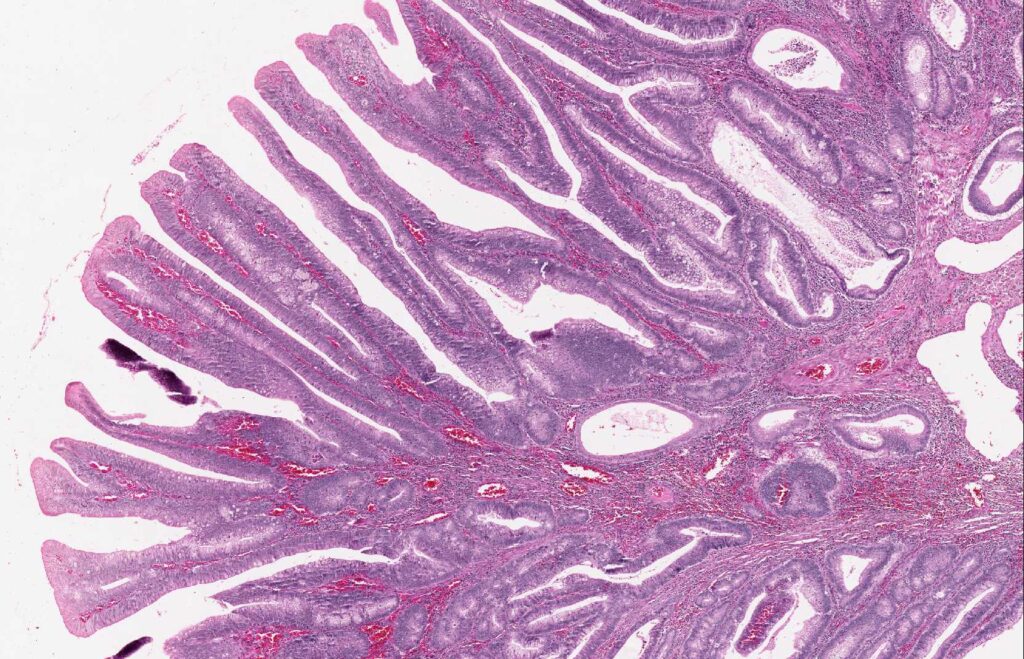
Villous Adenomas
- Often larger and sessile
- Covered by finger-like (villous) projections
- Malignancy risk: Highest among adenomas
- Appearance: May appear shaggy or cauliflower-like
Tubulovillous Adenomas
- Features of both tubular and villous types
- Malignancy risk: Intermediate (increases with the amount of villous architecture present)
Invasion and Malignancy Potential
When dysplastic epithelial cells invade the lamina propria, the lesion becomes an intramucosal carcinoma. However, true malignancy is only diagnosed when the cells breach the muscularis mucosa and enter the submucosa:
Invasive adenocarcinoma: Invades beyond muscularis mucosa; potential for metastasis
Intramucosal carcinoma: Limited to mucosa; no lymphatic access; polypectomy is usually curative
Let’s pause for a second because this is really important – and I missed it the first (and second) time I heard it.
There are no working lymphatic vessels in the lamina propria (the layer just under the colon epithelial lining). That means if a cancer starts in the colon and breaks through the basement membrane into the lamina propria, it still can’t spread anywhere else yet. There’s no way out—no lymphatics means no escape route for the cancer cells.
For the cancer to keep spreading, it has to push deeper into the next layer, called the muscularis mucosa. Once it gets through that layer, then it can reach the lymphatic system and might spread. At that point, doctors may need to do a bigger surgery and check nearby lymph nodes.
But if the cancer hasn’t made it past the lamina propria, removing it can actually cure the patient!

Key Risk Factors for Malignancy
- Size: Larger polyps are more likely to be malignant
- <1 cm: Rarely malignant
- 4 cm: ~40% contain invasive cancer
- Histology: Villous > Tubulovillous > Tubular
- Growth pattern: Sessile > Pedunculated (in terms of risk)
- Number of polyps: Multiple or recurrent polyps increase overall risk
Study Tips
- Flat = sneakier but riskier
- Villous architecture is most associated with malignant potential
Use the mnemonic: “Villous = Villainous” to recall high malignancy risk.
- Bigger = badder: Size correlates with malignant potential (esp > 1cm)

Way cool! Some extremely valid points! I appreciate you penning this write-up and the rest of the website is also
really good.
Thank you for reading!
Highly descriptive article, I loved that a lot.
Will there be a part 2?
Thanks for reading! Is there a topic you’d be be interested in seeing more about?
Greetings! I’ve been following your weblog for a long time now and finally got the courage to go ahead and give you a
shout out from Atascocita Texas! Just wanted to say keep up the excellent work!
Nice to hear from you and thanks for saying hello!
you’ve got an incredible weblog right here! would you like to make some invite posts on my blog?
Good day! This post could not be written any better!
Reading this post reminds me of my good old room mate! He always kept chatting
about this. I will forward this article to him.
Fairly certain he will have a good read. Thank
you for sharing!
Thanks for every other informative site. Where else may I am getting that kind of information written in such a perfect approach?
I’ve a project that I am just now running on, and I’ve been on the
look out for such information.
Hello would you mind letting me know which webhost you’re using?
I’ve loaded your blog in 3 completely different browsers and
I must say this blog loads a lot quicker then most.
Can you recommend a good hosting provider at a fair price?
Thanks, I appreciate it!
I’m using Hostinger
Way cool! Some very valid points! I appreciate you writing this article and also the rest of the site is also
very good.
magnificent issues altogether, you simply won a emblem new reader.
What might you suggest in regards to your post that you made
a few days in the past? Any positive?
What’s up i am kavin, its my first occasion to commenting
anyplace, when i read this paragraph i thought i could also make comment due to this brilliant piece of writing.
Hey Kavin thanks for reading!
Hello! I could have sworn I’ve been to this blog before but after reading through some of the post I realized it’s new to me. Anyhow, I’m definitely happy I found it and I’ll be bookmarking and checking back frequently!
Pingback: What Is a Pathologists’ Assistant? A Complete Guide to the PA Role